Your cardiovascular system, comprised of the heart and a vast network of blood vessels, keeps every part of your body supplied with oxygen and nutrients. When this system is disrupted by reduced blood flow or vessel damage, the effects can be severe.
Cardiovascular disease (CVD) progresses silently, with few or no early symptoms. By the time signs appear, serious damage may already be present. According to the CDC, coronary heart disease caused 371,506 deaths in 2022, and each year, about 805,000 Americans experience a heart attack.
Comprehensive cardiovascular testing helps detect risk factors and structural heart issues early, allowing for timely intervention and informed treatment decisions. In this guide, we’ll walk you through the types of tests involved, what each one reveals, and how you can prepare for them.
While testing isn't necessary for everyone, certain individuals may benefit more than others. You might be advised to undergo cardiovascular assessments if:
Smoking is still one of the biggest preventable threats to public health. Its long-term damage to the heart and blood vessels is well known. Research shows that more than 30% of deaths from coronary heart disease are linked to smoking, whether from smoking directly or being exposed to secondhand smoke.
According to the World Health Organization, smoking is responsible for about 10% of all cardiovascular diseases worldwide.
Extra pounds can lead to increased pressure on your heart and often goes hand-in-hand with conditions like high blood pressure or elevated cholesterol, both of which increase cardiovascular risk. In fact, about 70-80% of people with coronary artery disease are overweight or obese.
Diabetes, high blood pressure (hypertension), and elevated cholesterol can silently damage your blood vessels over time.
For example, high levels of LDL (or "bad") cholesterol can cause fatty buildup inside your arteries. This makes the arteries narrower and disrupts healthy circulation, leading to serious events such as strokes or heart attacks.
To find out if heart disease runs in your family, focus on two things:
If a close family member, like a parent or sibling, had a heart attack, stroke, or was diagnosed with heart disease before 55 in men and 65 in women, this could suggest an increased risk for you.
Chest discomfort, shortness of breath, feeling unusually tired or weak, or palpitations might be signs of an underlying heart condition.
As you get older, your chances of developing heart disease go up.
Autoimmune diseases are now known to raise the risk of CVDs, especially in women.
Conditions like rheumatoid arthritis and lupus cause long-term inflammation throughout the body. This can damage blood vessels, speed up the buildup of plaque, affect small blood vessels, and increase the risk of blood clots.
These diseases can affect many parts of the heart, not just the arteries. They may impact the heart muscle, valves, outer lining, or even the heart's electrical system.
A large study in the UK found that people with autoimmune conditions had a 56% higher risk of cardiovascular events compared to those without these conditions. Among the 19 autoimmune diseases included in the study, systemic sclerosis showed the strongest association, with more than three times the usual risk.
Even if you're asymptomatic, a cardiovascular screening could reveal early issues that can be managed before they become serious.
These tips apply across any cardiovascular tests and can help prevent delays or inaccurate results:
Include all prescription drugs, over-the-counter medications, vitamins, and herbal supplements. Note the dose and frequency of each item. Certain medications may need to be paused or adjusted before testing, so your care team needs accurate information.
Some cardiovascular tests involve exposure to radiation or contrast agents that may not be recommended during pregnancy. Always let your provider know in advance, even if you’re only possibly pregnant.
Alert your care team to any allergies, especially to:
This helps avoid complications during procedures that use injected agents or adhesive materials.
Be ready to discuss:
Tell your provider if you have:
Some tests, like MRIs, may be affected by or unsafe with certain implants.
There’s no single test that gives a full picture of your cardiovascular health. Instead, doctors use a combination of exams based on your symptoms, history, and overall risk profile.
Here’s a breakdown of the most widely used tests in cardiovascular medicine:
These are the first tests your doctor will usually do to spot early signs of heart disease or risk factors:
Blood pressure is measured using a device called a sphygmomanometer, which can be manual or digital. A cuff is wrapped around your upper arm, and it inflates to temporarily stop blood flow in your artery.
As the cuff slowly deflates, the device detects the pressure in your arteries. It’s measured in two numbers–systolic (top number) and diastolic (bottom number), and the reading is shown as systolic/diastolic (e.g., 120/80 mmHg).
Here's what the levels mean:
For the most accurate reading, avoid caffeine, smoking, or exercise for 30 minutes beforehand, and sit quietly for 5 minutes before being measured.
If you see your doctor regularly for checkups, they may check your blood pressure at each visit. If you don’t go often but your levels are in the normal range, checking them at least once a year is usually enough.
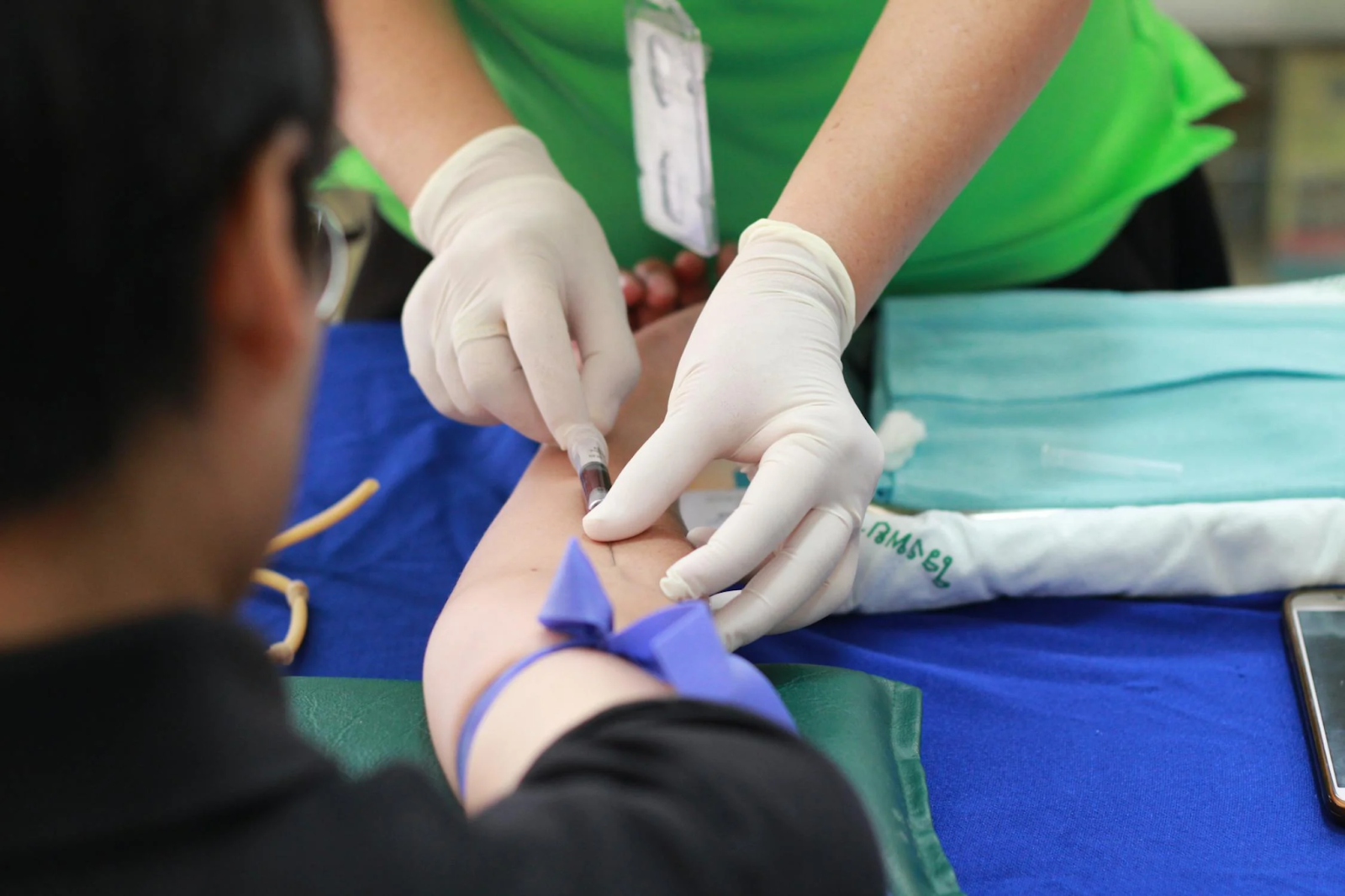
You should have your cholesterol levels checked starting at the age of 20. This can be done with either a fasting or non-fasting blood test. The test will measure:
Once you turn 40, they may also use a calculator to estimate your 10-year risk of having a heart attack or stroke.
For a fasting blood test, don’t eat or drink anything except water for 8 to 12 hours before your appointment. Avoid alcohol and high-fat foods the day before. Wear short sleeves or something with sleeves you can easily roll up. If you’re nervous about blood draws, tell the staff.
Get tested every 4 to 6 years if you’re at normal risk. If your doctor says you’re at higher risk for heart disease or stroke, you’ll need testing more often.
According to the American Diabetes Association, you should get your blood glucose tested starting at age 35. It’s usually tested in one of the following ways:
Here are the general ranges:
For Fasting Glucose and OGTT:
For the HbA1c test, no fasting is needed. You can eat and drink normally before this test.
In all cases, wear loose-fitting clothing that makes it easy to access your arm for the blood draw.
If you’re healthy and not diabetic, get your blood glucose tested at least once every 3 years. However, if you have risk factors, like being overweight, having high blood pressure, or a family history of diabetes, your doctor may recommend more frequent testing.
This blood test checks for very small increases in a protein called C-reactive protein (CRP), which is made by your liver. Under normal conditions, CRP levels in the blood are low. But when your body is inflamed, your liver releases more CRP into your bloodstream. An increase in CRP can point to inflammation or a potentially serious condition.
The high-sensitivity CRP (hs-CRP) test is a more advanced version of the standard CRP test. While a standard CRP test measures CRP levels from 8 to 1,000 mg/L, the hs-CRP test measures much smaller amounts, from 0.3 to 10 mg/L.
The test results are usually interpreted as:
There is no universal rule on when to get the hs-CRP test. However, organizations like the AHA and the CDC suggest it may be helpful for people with a moderate (10-20%) risk of having a heart attack within 10 years.
No special preparation is usually needed for an hs-CRP test. However, chronic inflammatory conditions like arthritis can raise CRP levels on their own, making the test less useful for predicting heart disease risk in those cases. Discuss these factors with your doctor so they can give you the most accurate assessment.
There are no official guidelines on how often to take the hs-CRP test. However, because CRP levels can change over time, doctors usually base risk assessments on the average of two tests. These are typically done about two weeks apart, ideally when you're not sick or dealing with any infections.
If early screening shows signs of cardiovascular disease or reveals risk factors, your doctor may order these next:
ECG (also called an EKG) is quick, noninvasive, inexpensive, and provides an immediate snapshot of your heart's electrical activity. It shows how fast your heart is beating, whether the rhythm is normal or irregular, and how well the signals move through the heart.
During the test, you'll lie down while small sticky patches (electrodes) are placed on your chest, arms, and legs. These connect to a machine that prints out your heart’s activity. The whole test only takes a few minutes.
Key elements of ECG interpretation include:
Avoid lotions or oils on your skin. Moisturizers, body oils, or powders on your chest can interfere with the electrode's ability to stick properly and may affect the signal quality. Also note that if you have a lot of hair on your chest, arms, or legs, the technician may need to shave small areas to help the electrodes stick properly.
If your ECG shows something unusual, your doctor might order a heart imaging test to see more clearly how your heart is working. One of the most common first steps is a transthoracic echocardiogram (TTE).
A TTE is a standard, noninvasive test that uses high-frequency sound waves (ultrasound) to create real-time images of your heart.
During the procedure, a small handheld device called a transducer is gently moved across your chest. Sound waves from the device strike the heart and return as echoes, which are then processed into images.
The test provides essential details such as:
The test typically takes about 30 to 60 minutes to complete.
Preparation is generally simple and minimal. It’s a good idea to wear comfortable, loose-fitting clothing since you’ll be asked to undress from the waist up. You’ll be given a gown to wear during the procedure. Avoid using lotions, powders, or oils on your chest, as they might interfere with the ultrasound gel and affect image quality.

A stress test shows how well your heart handles physical activity. Some heart issues only appear when your heart is working harder, like during exercise. If your resting ECG looks normal or close to normal and you're able to exercise, this is often the first test your doctor will recommend.
Stress tests come in various forms, broadly categorized as exercise-based or pharmacological (medication-induced). If you can’t exercise, your doctor will give you medicine through an IV over 10 to 20 minutes that makes your heart beat faster, similar to how it would during physical activity.
Before starting either type of test, your doctor will place electrodes on your chest to monitor your heart. You’ll also have a blood pressure cuff on your arm and a pulse sensor on your finger. These help track your heart activity and blood pressure.
During the exercise-based stress test, most people use a treadmill or a stationary bike. The most common routine used is the Bruce protocol. Each stage lasts three minutes and gets a bit harder than the last. Most people exercise for about 6 to 12 minutes, depending on what their body can handle.
If your heart rate and blood pressure rise normally and there are no ECG changes or symptoms, your test is likely normal.
Your doctor might also calculate a Duke Treadmill Score (DTS). This score (typically ranging from +15 to -25) combines your exercise time, any ECG changes, and whether you experienced chest pain to estimate your future heart risk:
Scores in the middle range usually mean more imaging is needed for a clearer diagnosis.
On the day of your test, you may be asked to skip certain medications or avoid caffeine, like coffee or tea, since these can affect the results. Be sure to wear comfortable clothes and shoes.
There are times when this test could be risky. Your doctor will avoid the test completely if you:

Cardiac MRI uses magnets and radio waves to take clear, detailed pictures of your heart. Compared to a cardiac CT scan, it shows a stronger contrast between tissues and blood vessels, which helps doctors see the heart in more detail.
Like a CT scan, you’ll lie on a table that moves into a tunnel-like machine. Sometimes, a contrast dye will be injected into your arm to help highlight the images. You’ll hear loud humming or tapping noises and may be asked to hold your breath for a few seconds at a time. It usually takes about 30 to 60 minutes.
Because the MRI uses a strong magnet, avoid wearing metal objects, including jewelry, watches, hairpins, or hearing aids.
This quick and painless test uses ultrasound technology to examine the carotid arteries, which are blood vessels found in the neck responsible for supplying blood to the brain.
During the test, you’ll lie on an exam table while a technician applies a small amount of gel to your neck. A transducer is then moved along your neck to capture detailed images of the arteries. The whole process typically takes 15 to 30 minutes.
This test is safe and noninvasive. It uses no radiation, just harmless sound waves, similar to the ones used in pregnancy ultrasounds.
Avoid high-collar clothing or turtlenecks so your neck is easily accessible. Don’t apply lotions, oils, or powders to your neck on the day of the exam. You may also be asked to remove necklaces or earrings that could obstruct the area.
This specialized test is used when your doctor suspects blockages in the arteries that supply your heart. It’s widely considered the gold standard for diagnosing coronary artery disease.
You’ll be sedated during the procedure to help you relax. The doctor will make a small incision in your wrist or groin to insert a catheter, which is then guided to your heart. Once it’s in the right spot, a contrast dye is injected through the catheter, and X-ray images are taken to see how blood flows through your heart’s arteries. Areas where the dye doesn’t flow well may point to a blockage.
The procedure usually takes about an hour, but may take longer if other treatments are done. If a blockage is found, the doctor may use a balloon (angioplasty) and possibly place a stent to open the artery during the same session.
You’ll be asked to fast for 6 to 8 hours before the procedure. Arrange for someone to drive you home after the test since you’ll be sedated and unable to drive.
This is a variation of the standard transthoracic echocardiogram. Instead of placing the transducer on your chest, the doctor gently guides it down your throat and into your esophagus. For this test, you’ll need to be sedated and have a numbing spray for your throat.
TEE is typically used when doctors need a closer, more detailed view of the heart. Because the probe is placed in the esophagus, right behind the heart, there’s less interference from the chest wall, muscles, and ribs. The test may take up to 90 minutes.
Do not eat or drink anything for at least 6 hours before the test. You’ll receive sedation through an IV, so arrange for someone to drive you home.
Comprehensive cardiovascular testing provides valuable insight into your heart health. It goes beyond routine measurements, helping guide decisions that support long-term well-being.
If it’s been years since your last heart check, or if you're experiencing unexplained symptoms, it may be a good time to talk with your doctor. Getting the right test at the right time can help catch potential issues early and guide appropriate care.